The pandemic has made it clear that fee-for-service is unsustainable, and we’re fully committed to value-based care as the solution to stabilizing Vermont’s increasing health care costs.
We begin this year thankful for the collective courage, dedication, and resilience of Vermont’s health care providers toward combating the spread of COVID-19 while continuing to provide essential services. We are also grateful for our community of providers who have continued to transform health care delivery by improving health outcomes, quality of care, and containing cost growth.
2020 was a challenging year for many—with a unique strain on our health care system and Vermonters providing care. It has also highlighted, more than ever, how vulnerable our providers are under the fee-for-service model. Throughout 2020 and into 2021, OneCare Vermont continues to lead the transition away from fee-for-service to value-based care and improved outcomes for communities in Vermont through data analytics, a statewide care model, and payment reform. Below is a quick overview of what OneCare did in 2020 to support providers and communities, respond to the pandemic, and move forward with health care reform efforts.

Ensured Cash Flow to Practices:
When the pandemic hit Vermont, the healthcare provider community faced unprecedented operational challenges and financial strains. OneCare aggressively searched for ways to provide financial relief to providers. We were able to advance payments to primary care practices, home health, designated agencies, and area agencies on aging, as well return Value-Based Incentive Fund payments to hospitals. Read more about our direct support to providers & healthcare organizations.
Gathered Data to Identify the Most Vulnerable:
The pandemic highlighted significant gaps in health care and a heightened need to leverage health data analytics in order to identify people with complex needs and/or at high risk due to housing issues, food insecurity, loss of income, and other criteria. OneCare's analytics team rose to the challenge and developed the COVID-19 Care Coordination Prioritization Application so providers could identify and proactively reach out to patients with the greatest COVID-19 virus risk. Read more about the other innovative ways in 2020 OneCare made it possible for technology and data to respond to health care needs.

Strengthened Statewide Care Coordination Model & Offerings:
Care coordination plays an important role in OneCare’s work to improve health outcomes for Vermonters while stabilizing health care costs. In September, OneCare met the goal of achieving an all-payer blended 15% care managed rate with 4,178 Vermonters who became actively care managed. Learn more about our successes in care coordination and watch “Fred’s Story.”

Provided New Online and Socially Distanced Prevention Supports for Individuals and Groups in Local Communities:
RiseVT, OneCare’s primary prevention program, adapted from in-person programming to virtual offerings and focused on investments in outdoor recreation spaces and initiatives. While local program managers amplified efforts to improve trails, distribute emergency food, and support families, the RiseVT statewide team administered several virtual campaigns to encourage healthy lifestyles for physical and mental health. Learn more about these initiatives as well as the DULCE program which addresses health in infants 0-6 months.

Advanced Health Care Payment Reform:
As OneCare adapted and responded to the needs of our health care community to get through this unprecedented time, we simultaneously worked to stay on track with our goal to move away from fee-for-service toward value-based care. From policy briefings to media highlights to legislation, learn more about how we continued to work toward our goal of payment reform.

Ensured Cash Flow to Practices:
When the pandemic hit Vermont, the healthcare provider community faced unprecedented operational challenges and financial strains. OneCare aggressively searched for ways to provide financial relief to providers. We were able to advance payments to primary care practices, home health, designated agencies and area agencies on aging, as well return Value-Based Incentive Fund payments to hospitals. Read more about our direct support to providers & healthcare organizations.
Gathered Data to Identify the Most Vulnerable:
The pandemic highlighted significant gaps in health care and a heightened need to leverage health data analytics in order to identify people with complex needs and/or at high risk due to housing issues, food insecurity, loss of income, and other criteria. OneCare's analytics team rose to the challenge and developed the COVID-19 Care Coordination Prioritization Application so providers could identify and proactively reach out to patients with the greatest COVID-19 virus risk. Read more about the other innovative ways in 2020 OneCare made it possible for technology and data to respond to health care needs.

Strengthened Statewide Care Coordination Model & Offerings:
Care coordination plays an important role in OneCare’s work to improve health outcomes for Vermonters while stabilizing health care costs. In September, OneCare met the goal of achieving an all-payer blended 15% care managed rate with 4,178 Vermonters who became actively care managed. Learn more about our successes in care coordination and watch “Fred’s Story.”

Provided New Online and Socially Distanced Prevention Supports for Individuals and Groups in Local Communities:
RiseVT, OneCare’s primary prevention program, adapted from in-person programming to virtual offerings and focused on investments in outdoor recreation spaces and initiatives. While local program managers amplified efforts to improve trails, distribute emergency food, and support families, the RiseVT statewide team administered several virtual campaigns to encourage healthy lifestyles for physical and mental health. Learn more about these initiatives as well as the DULCE program which addresses health in infants 0-6 months.

Advanced Health Care Payment Reform:
As OneCare adapted and responded to the needs of our health care community to get through this unprecedented time, we simultaneously worked to stay on track with our goal to move away from fee-for-service toward value-based care. From policy briefings to media highlights to legislation, learn more about how we continued to work toward our goal of payment reform.

Provided Direct Support and Ensured Cash Flow to Health Care Providers and Organizations
When the pandemic hit Vermont, the health care provider community faced unprecedented operational challenges and financial strains. OneCare aggressively searched for ways to provide financial relief to providers. We were able to advance payments to primary care practices, home health, designated agencies, and area agencies on aging, as well return Value-Based Incentive Fund payments to hospitals.
Predictable cash flow helps health care organizations continue to provide necessary services to their communities, especially during uncertain times. We continue to explore opportunities to increase participation in fixed payment programs to expand this value.
More highlights:
- Center for Health Care Strategies, Inc. interviewed CEO Vicki Loner about OneCare’s COVID-19 response. The interview focused on the rapid ramp-up of telehealth capacity in Vermont and how payment reforms in the state supported the ACO’s ability to take action swiftly.
- OneCare expanded the Comprehensive Payment Reform (CPR) program to support independent primary care practices.
- During the pandemic, we advocated at the federal, state, and payer level to reduce administrative burden, pressed for continued expansion of telehealth, and asked that providers be held harmless for performance and financial related penalties for the duration of the public health emergency.
- In March, CEO Vicki Loner penned a letter urging leaders to provide support and relief for clinicians and organizations that are part of Advanced Alternative Payment Models as they continue to serve on the front lines of the COVID-19 pandemic. In April, Loner also presented OneCare’s specific efforts to the Green Mountain Care Board.
- In late April, OneCare contributed to a letter that All Payer Model agreement signers sent to Medicare & Medicaid Innovation asking for specific actions that would support providers participating in the model during the pandemic.
- In support of our partners and the health care community, OneCare shared important public health messages and resources from partners on our social media outlets. We launched a campaign targeted at those who might have been delaying preventive care. We also created a public resources page with curated resources centered primarily around mental health, suicide prevention, and the pandemic.

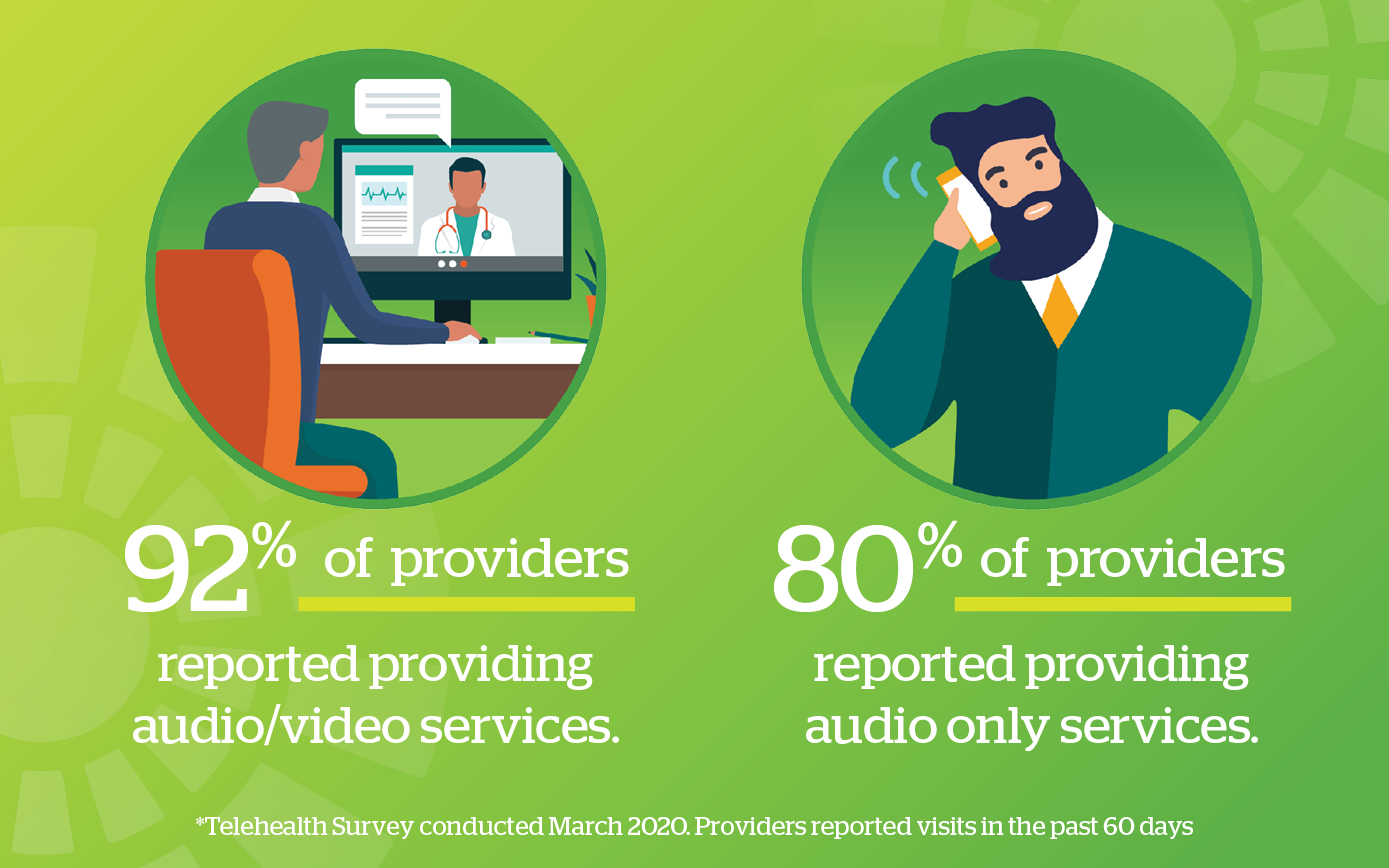
Gathered Data to Identify the Most Vulnerable
The pandemic highlighted significant gaps in health care and a heightened need to leverage health data analytics in order to identify those with complex needs and/or at high risk due to certain criteria such as social determinants of health. OneCare’s analytics team rose to the challenge and developed the COVID-19 Care Coordination Prioritization Application, so providers could identify and proactively reach out to patients with the greatest COVID-19 virus risk. The use of telehealth in both urban and rural areas accelerated as providers searched for ways to provide critically needed care services and to broaden reach in underserved areas. OneCare turned to its community of providers to find out telehealth’s potential impact on caring for Vermonters, and advocated for expanding the use of telehealth in routine medical care.
More highlights:
- Within weeks of the Governor’s announcement of the public health emergency, OneCare’s analytics team rapidly developed and launched the COVID-19 Care Coordination Prioritization Application, designed to help providers identify and proactively reach out to patients with the greatest COVID-19 virus risk, according to criteria advanced by World Health Organization, Centers for Disease Control and Prevention, and Johns Hopkins. The application has been profiled by several prominent local and national organizations. The analytics team also developed an Influenza Vaccine App to help providers identify and reach out to as many high-risk Vermonters as possible who had not yet received a flu shot.
- The use of telehealth rose rapidly in Vermont communities and became the new normal as providers adapted quickly to provide care for patients during the COVID-19 pandemic. In a statewide survey conducted by OneCare Vermont in March, health care providers overwhelmingly responded that they were providing telemedicine services to patients during the public health emergency. Learn more in our blog post about the survey results.
- OneCare regularly participated in the Vermont Program for Quality in Healthcare Quality Inc. telehealth weekly office hours that ran from spring to fall.
- OneCare advocated for the value of telehealth: Several of our educational sessions covered telehealth, available on our clinical education page. OneCare Chief Medical Officer Dr. Norman Ward penned an op-ed, published in the Barre-Montpelier Times Argus, explaining why telehealth is essential to health equity and healthcare access. We also posted a Q&A with Dr. Ward where he shared his viewpoints on annual wellness visits via telehealth.
- OneCare was also a participating stakeholder in the workgroup convened by the Department of Financial Regulation that was tasked to draft a report of recommendations around telehealth coverage to the legislature. CEO Vicki Loner submitted a letter of support for continued expansion of telehealth services in Vermont on behalf of OneCare.
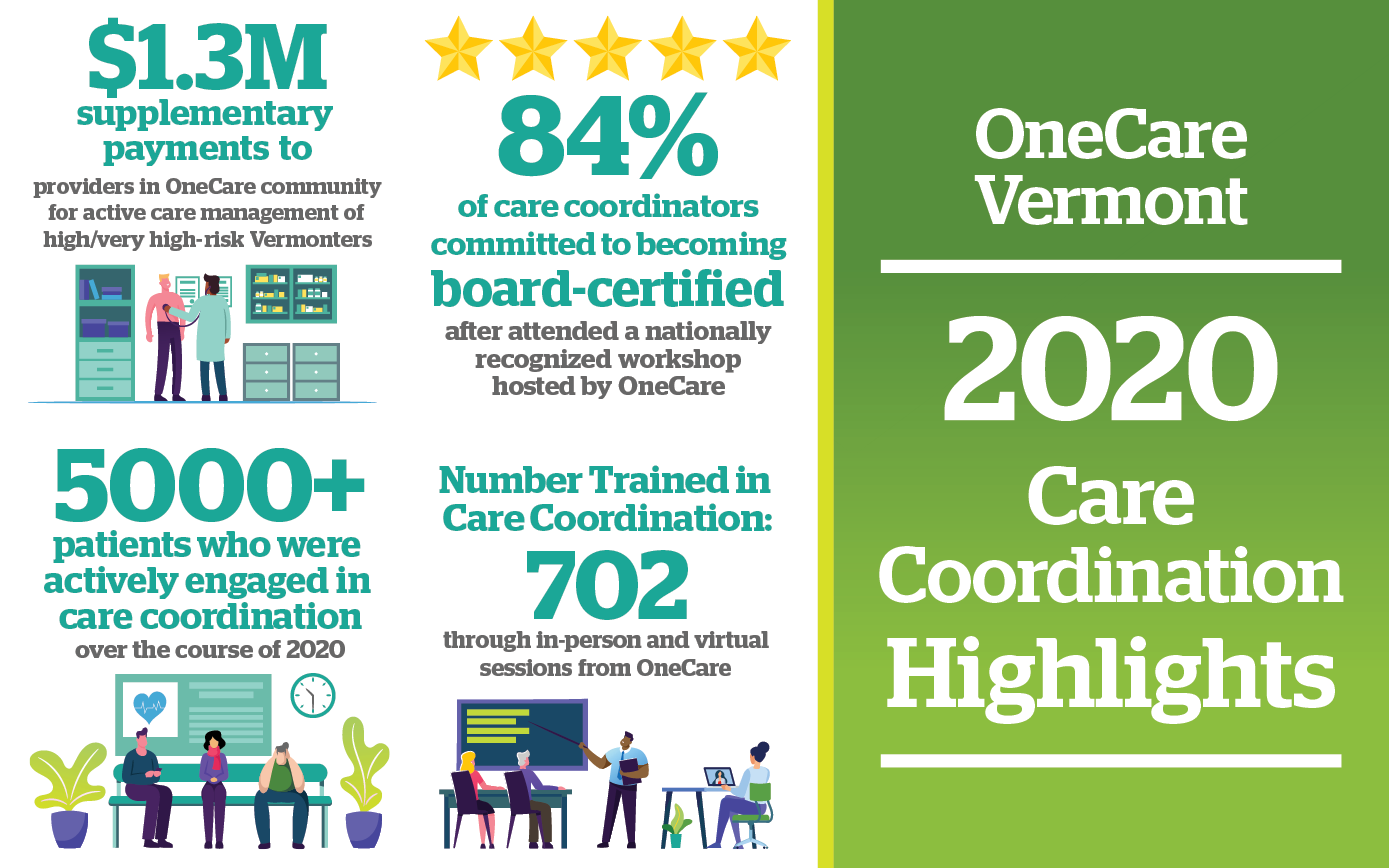
Strengthened Statewide Care Coordination Model & Offerings
Care coordination plays an important role in OneCare’s goals to improve health outcomes for Vermonters while stabilizing health care costs. In September, OneCare met the goal of achieving an all-payer blended 15% care managed rate with 4,178 Vermonters who became care managed. Through the hard work of care management teams statewide, OneCare achieved active care coordination of 5,000+ Vermonters* in 2020.
Other highlights:
- Watch Fred’s story: an example of care coordination that tells the story of how Fred’s care team worked together to improve Fred’s health outcomes. Fred’s total cost of care was reduced by 97% after one year of outreach.
- The official launch of Vermont Health Learn, an e-learning system to centralize educational offerings for OneCare and its statewide partners, was timely during the pandemic when virtual learning was crucial.
- To support overall advancement of care coordination in Vermont, OneCare continued to virtually provide clinical education sessions throughout the year, available to both health care providers and the general public. Dr. Mark Levine even joined us as a special guest presenter for our session entitled “COVID-19 Update & Impact on those with Respiratory Conditions,” available on our clinical education page.
- OneCare’s Care Coordination Team also offered a series of educational events dedicated to effectively coordinating care for complex patients.
- Jodi Frei, manager of clinical programs at OneCare, was interviewed in a Policy in Plainer English podcast that also dives into the topic of care coordination.
*The total number of Vermonters who receive the services of a care management team fluctuates throughout the year as they become actively care managed, or when their care management is completed or ended.

Provided New Online and Socially Distanced Prevention Supports for Individuals and Groups in Local Communities:
RiseVT, OneCare’s primary prevention program, adapted from in-person programming to virtual offerings and focused on investments in outdoor recreation spaces and initiatives. While local program managers amplified efforts to improve trails, distribute emergency food, and support families, the RiseVT statewide team administered several virtual campaigns to encourage healthy lifestyles for physical and mental health:
- We’ve Got You, a daily round-up of resources and tips to support individuals during the initial Stay Home, Stay Safe order;
- Rise to 5K, a 10-week training program designed to help people prepare for a 5K run/walk;
- Rise & Walk, encouraging participants to increase their activity through walking while learning healthy lifestyle tips from local health care providers; and
- Rise & Tae Kwon Do for middle school students, and What’s Your Calm mindfulness campaign.
RiseVT also completed projects ranging from infrastructure development to promoting walkable communities, expansion of bike and walking paths, health education programming, and broadening access to local wellness initiatives.
To offer preventive health care to our youngest citizens, Developmental Understanding and Legal Collaboration for Everyone (DULCE) is an intervention model that takes place within pediatric care offices to address health in infants ages zero to six months and to provide parental support. OneCare helped expand new DULCE sites in 2019 and these sites are currently working to expand the program and further integrate within pediatric practices. One of these family specialists, Danielle Patrick, remarked on her experience within DULCE during the pandemic: “In the past year since enrolling my first family in October 2019, I have worked remote more than I have been in the pediatric office. As much as I have missed the in-person interactions with DULCE families, I am thankful that I have been able to continue to support families while their needs have increased due to the pandemic. I have been seeing a rise in mental health needs and have been able to offer families the opportunity to take part in a virtual support group for mothers that I have been co-facilitating.” And read about the impact that DULCE has had on The Family Place in Norwich, Vermont.
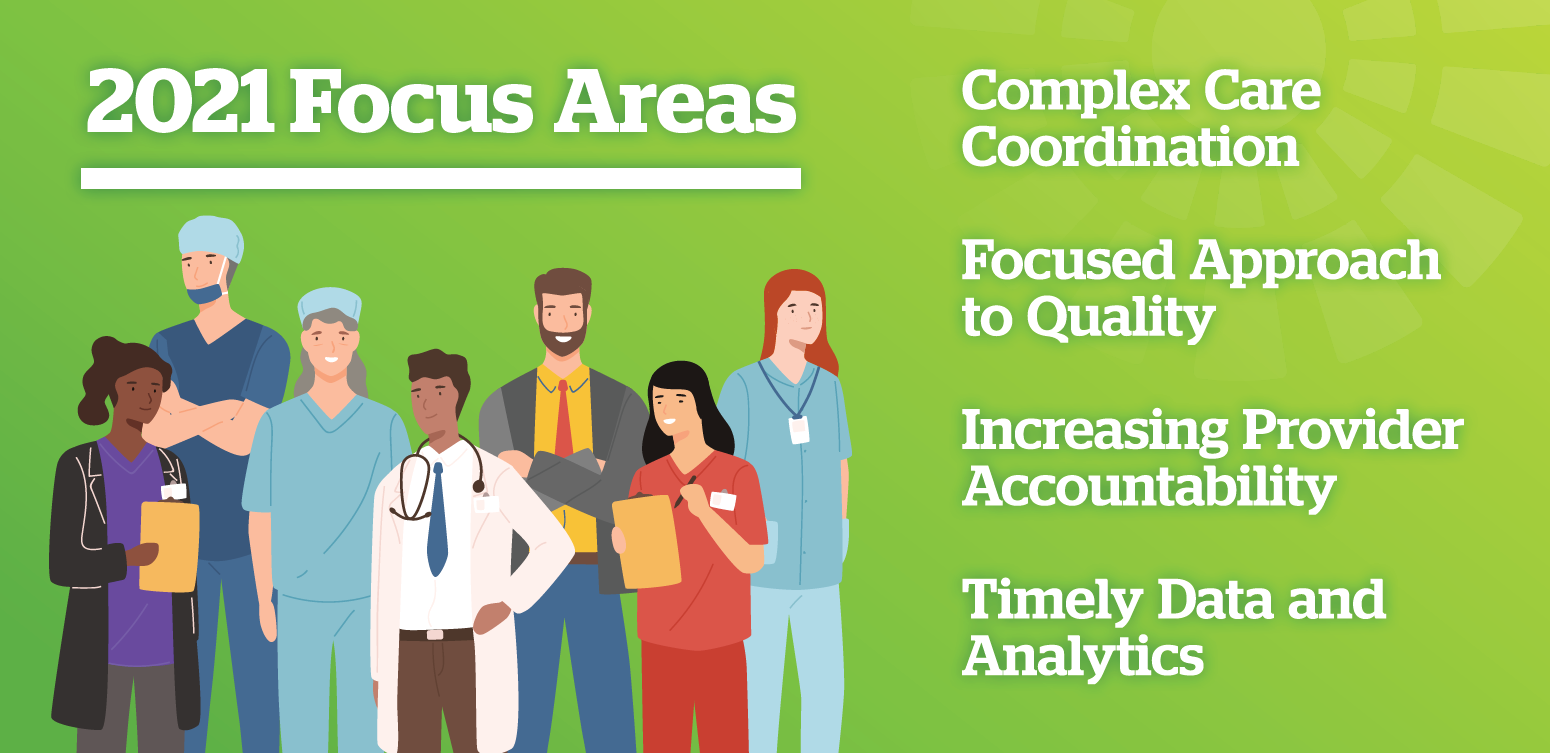
Advanced Health Care Payment Reform
While OneCare pivoted and responded to the needs of our health care community to get through this unprecedented time, we simultaneously worked to stay on track with our goals to moving away from fee-for-service toward value-based care. Highlights include:
- In June, CEO Vicki Loner was interviewed by WCAX-TV in a feature piece that describes how the move to fixed payments has helped keep hospitals and providers buoyant during times of crisis, especially the COVID-19 public health emergency.
- The Value in Health Care Act was introduced, which supports value-based health care reform initiatives. An analysis of this bill is available here. The National Association of ACOs also created a section-by-section summary – a quick guide for anyone interested in how this bill will benefit ACOs and Alternative Payment Models.
- In June, the Duke-Margolis Center for Health Policy released an issue brief describing the positive impact of value-based payments on health organizations during the pandemic. CEO Vicki Loner was interviewed and contributed to the brief which explores how health care delivery organizations were able to leverage value-based payment models to respond to the pandemic and support COVID-19 detection and containment. The brief was released in conjunction with a national webinar on payment reform.
- In September, the Commonwealth Fund published a case study of independent primary care practices that provide much-needed care in their communities, including the Thomas Chittenden Health Center in Williston, Vermont. Dr. Joseph Haddock said population health management payments from OneCare Vermont provided stability during the pandemic and have enabled the practice to hire additional staff and offer more services.
- We posted quality measure and scorecard results from 2019, which can be viewed on our results page, and reported that OneCare providers earned $11.3 million in Medicare shared savings.
- In October, we released our 2019 Annual Report, representing a snapshot of 2019’s progress, results, and outcomes.
- OneCare’s 2021 network was finalized at the end of September, adding the Rutland region to the Medicare program and anticipating an overall 28,000 new Vermonters who will receive care from providers participating in OneCare.
- We presented our 2021 budget to the Green Mountain Care Board in late October as part of OneCare’s annual budget and certification process. The budget supports the cooperative effort of thousands of providers across Vermont to stabilize health care costs and improve health for Vermonters.
- In December, OneCare was one more than 500 ACOs, health systems, and medical practices that submitted a letter to Congress to freeze Advanced Alternative Payment Models bonus thresholds at their current levels for 2021 and 2022. Congress agreed and the language was included in the final COVID-19 relief funding bill which was approved on December 21.