OneCare’s care coordination model supports care teams in communities across Vermont.
Care coordination requires a strong relationship between the patient, their primary care provider, and other members of a person’s care team. OneCare provides tools and resources to help facilitate this coordination. With OneCare tools and support, providers work together across organizations to help patients access the care they need and avoid expensive duplicate services. Providers share information about what is happening with the patients they are all caring for—if the person is admitted or discharged from the hospital, if social or economic factors put patients at risk, or if a change in their mental health has occurred. That way, providers caring for the same patient can quickly identify ways to address their needs and the patient only has to tell their story once.
OneCare provides the following to support care coordination:
- Data to help inform primary care providers which patients on their panel may benefit from care coordination
- Best practices and tools for forming a community- and team-based care coordination model
- Secure communication tools care coordination team members can use no matter where they work
- Training for health care workers and partners statewide on care coordination processes and procedure
Population Health Approach: A plan for every person
OneCare uses data to identify individuals whose well-being may be at risk due to their health conditions. This information is provided to communities to review and connect with individuals who may benefit from enhanced coordination of care. The goal is to identify the care and resources that are needed to help individuals meet their health goals.
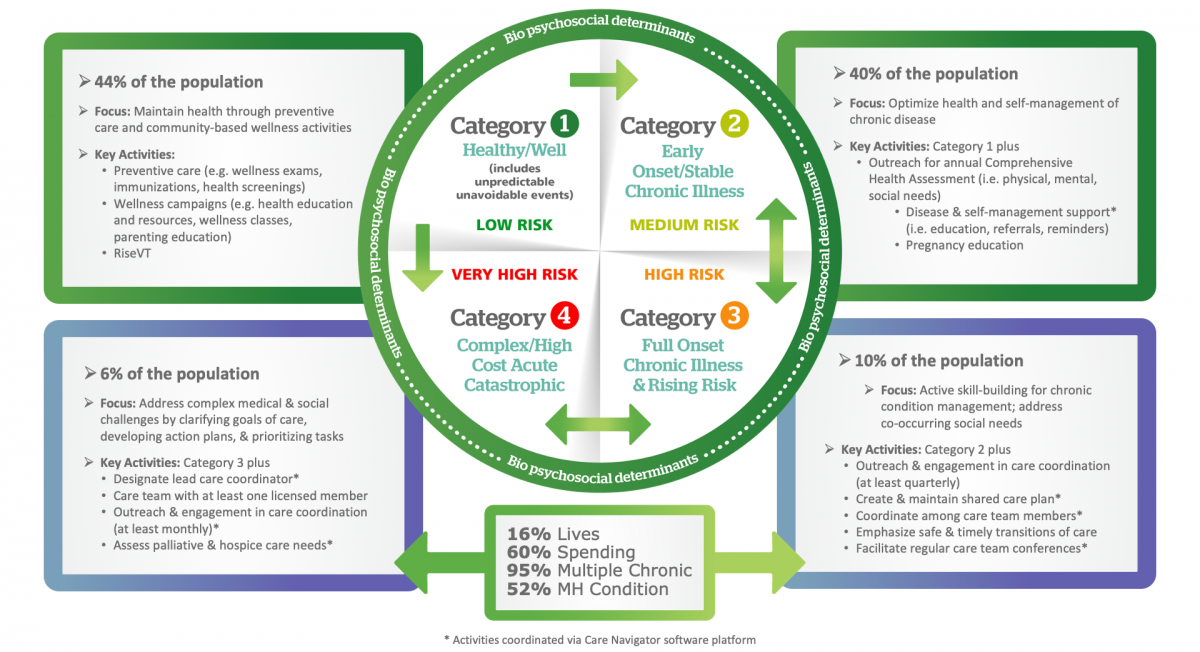
Care Coordination activities promote holistic and person-centered care to ensure that an individual’s needs and goals are understood and shared among providers, patients, families, and team members.
The ultimate aim is to improve the quality of care, the patient experience of care and the patient engagement in their plan of care as they interact with health care providers. OneCare supports a community-based care coordination program for all attributed beneficiaries. Care coordination services are guided by the use of assessments that evaluate the individual’s physical health, mental health, and social needs and desires to support the attainment of optimal health. OneCare’s care coordination model actively promotes a holistic and person-centered approach to care delivery, ensuring that all team members participating in an individual care team can identify and support the individual’s preferences and needs.
Care coordination streamlines care for the patient by reducing the redundancy in visits, facilitating access to specialty care and services, and allowing team members to share information about the patient. These supports allow the patient to focus on the achievement of health care goals knowing that all team members are informed.
OneCare follows the definition of Case Management outlined by the State of Vermont Care Models Care Management Workgroup:
“Programs that apply systems, science, incentives, and information to improve services and outcomes in order to assist individuals and their support system to become engaged in a collaborative process designed to manage medical, social, and mental health conditions more effectively. The goal of care management is to achieve an optimal level of wellness and improve coordination of care while providing cost-effective, evidence-based or promising innovative and non-duplicative services. It is understood that in order to support individuals and to strengthen community support systems, care management services need to be culturally competent, accessible, and personalized to meet the needs of each individual served.”
OneCare supports community-based care coordination services and enhanced communication and collaboration across care team members.
OneCare supports prevention-focused initiatives that promote health and wellness through a variety of strategies designed to impact individuals, organizations, communities, as well as the overall health care delivery system.
OneCare supports primary care practices to identify those patients who may benefit from outreach for annual wellness exams and promotes the Vermont Department of Health offerings for wellness promotion in the community. Offerings such as: engaging maternal and child health coordinators to promote improved developmental screening in their communities through innovative partnerships with providers, early care and education professionals, and other service providers; collaborating with Parent-Child Centers on early childhood mental health and trauma interventions; expanding oral health strategies such as the application of fluoride varnish in primary care; improving vaccination rates; increasing physical activity and nutrition; promoting safety and injury prevention; tobacco cessation; and mental health services.
The OneCare disease management program works to identify populations with chronic diseases that may benefit from more intensive care supports.
The disease management program is rooted in utilizing evidence-based medicine, educating the care team with the most up-to-date clinical guidelines, and working to ensure treatment consistency for targeted populations and conditions. The program is designed to improve health for those patients with chronic conditions by providing ongoing education as well as access to community resources, services, and supports that can help patients successfully manage their conditions. OneCare’s community-based care coordination program facilitates and empowers individuals to work with their multidisciplinary care team to prevent complications and achieve an optimal state of health.
OneCare puts a focus on the following conditions:
- Congestive Heart Failure
- Chronic Obstructive Pulmonary Disease
- Diabetes
- Coronary Artery Disease
- Hypertension
- Asthma
- Tobacco Use
- High-Risk Pregnancy
Partnering with existing community resources, self-management programs
Community Resources
Care Coordination Toolkit
OneCare has developed a care coordination toolkit to be a resource for coordinating care for patients with complex needs and to serve as a resource for existing case management programs to integrate best practices. This toolkit is reviewed and updated quarterly to ensure tools and best practices are up to date.
To access the OneCare Care Coordination Toolkit
