Quality Performance
Quality health care is safe, effective, patient-centered, timely, efficient, and equitable. At OneCare Vermont, our quality team has three core functions to support improved population health outcomes, while linking to incentive programs that stabilize health care spending:
- Capture OneCare network performance through annual reporting on standard, national quality measures
- Create and implement focused, high impact payment incentive programs to drive change on established quality measures.
- Facilitate targeted, data-driven quality improvement initiatives in partnership with our network participants.

Quality is the foundation that we really want to invest in to take our already high-value care to the next level.
Alicia Jacobs, MD
Practicing Physician at Colchester Family Medicine, Vice Chair and Associate Professor in Family Medicine at the Larner College of Medicine at the University of Vermont, and Physician Liaison for OneCare Vermont
1. Capturing Network Performance
Value of Monitoring Annual Quality Measures over Time
OneCare’s annual quality measures monitor network performance over time, tracking our progress on improving the quality of care delivered to Vermont.
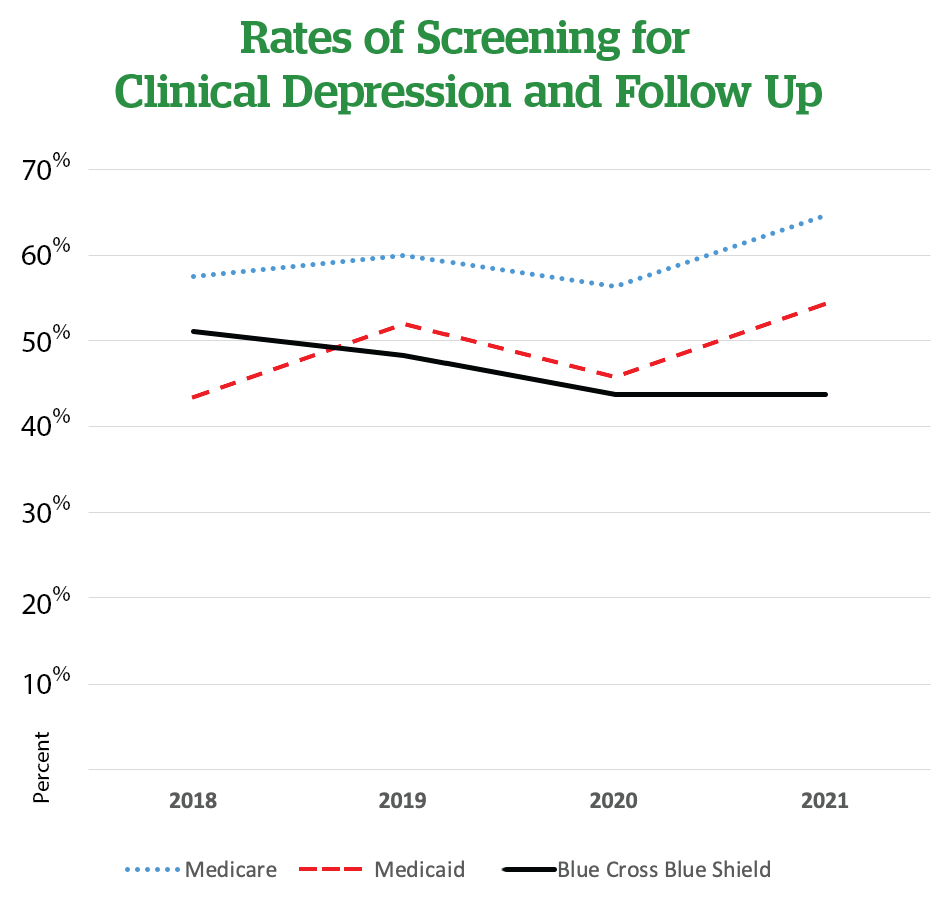
This chart, “Rates of Screening for Clinical Depression and Follow Up” is an example of monitoring a quality measure over time. The chart shows that, based on data from 2018 to 2021, rates of screening for clinical depression and follow up are generally increasing for two of OneCare’s payer programs: Medicare and Medicaid.
OneCare currently monitors 21 annual quality measures. These measures are established by Medicaid, Medicare, and MVP—payers OneCare contracts with on behalf of our network participants—and provide insights into the quality of care delivered by our network.
Our Annual Quality Measures Fall into These Categories:
Preventive Care for both Adults and Children
Screening for and Treatment of Chronic Disease
Treatment for Mental Health / Substance Use Disorder
Self Reported Patient and Caregiver Experience
Hospital Utilization
Annual Year-by-Year Quality Measures
Find details on select annual quality measures across all payers for which OneCare is contractually obligated to monitor, measure, and report on the performance of our network in improving quality of care delivered to Vermonters.
Medicare = Vermont Medicare ACO Initiative; Medicaid = Vermont Medicaid Next Generation; MVP QHP = MVP Qualified Health Plan; PHM Measure = Population Health Model Measure. Below the table, you’ll find an archive of prior year quality measures. Click on any of them to download and view them.
| 2024 Quality Measure | Medicare | Medicaid | Self-Funded | MVP QHP | PHM Measure |
|---|---|---|---|---|---|
| Follow-Up after discharge from the ED for Alcohol and Other Drug Dependence (30-Day) (NQF#2605) | Yes | - | - | - | - |
| Follow-Up after ED Visit for Substance Use - 30-Day (HEDIS FUA) | - | Yes | - | Yes | Yes |
| Follow-Up after ED Visit for Mental Illness -30 Day (HEDIS FUM) | - | Yes | - | Yes | Yes |
| Hospital-Wide, 30 Day, All Cause Unplanned Readmission (Quality ID#479) | Yes | - | - | - | - |
| Clinical and Clinican Group Risk-Standardized Acute-Admission Rate for Patients with Multiple Chronic Conditions (Quality ID#484) | Yes | - | - | - | - |
| Risk Standardized, Hospital Admission Rate for Patients with Multiple Chronic Conditions (18 and over) | - | Yes | - | - | - |
| Child and Adolescent Well-Care Visits 3-21 (HEDIS WCV) | - | Yes | Yes | Yes | Yes |
| Developmental Screening in the First Three Years of Life (CMS Child Core C-DEV) | - | Yes | Yes | - | Yes |
| ACO All-Cause Readmissions (HEDIS PCR) | - | - | - | Yes | - |
| Initiation of Alcohol and Other Drug Dependence Treatment (Quality ID# 305-Medicare Initiation of Substance Use Disorder Treatment (HEDIS IET- Medicaid, MVP, PHM) |
Yes | Yes | - | Yes | Yes |
| Engagement of Alcohol and Other Drug Dependence Treatment (Quality ID# 305-Medicare) Engagement of Substance Use Disorder Treatment (HEDIS IET-Medicaid, MVP, PHM) |
Yes | Yes | - | Yes | Yes |
| Follow Up after ED Visits for Patients with Mulitiple Chronic Conditions (HEDIS FMC) | - | - | Yes | - | Yes |
| Follow-Up After Hospitalization for Mental Illness (7 Days) (HEDIS FUH) | - | Yes | - | Yes | Yes |
| Breast Cancer Screening (HEDIS BCS-E) | - | - | - | Yes | - |
| Cervical Cancer Screening (HEDIS CCS-E) | - | - | - | Yes | - |
| Medicare Annual Wellness Visit | - | - | - | - | Yes |
| Influenza Immunization (Quality ID# 110) | Yes | - | - | - | - |
| Colorectal Cancer Screening (Quality ID# 113, HEDIS COL-E) | Yes | - | Yes | Yes | - |
| Tobacco Use Assessment and Cessation Intervention (Quality ID# 226) | Yes | Yes | - | - | - |
| Screening for Clinical Depression and Follow-Up Plan (Quality ID# 134) | Yes | Yes | - | - | - |
| Diabetes HbA1c Poor Control (>9.0%) (Quality ID#001) | Yes | - | - | - | - |
| Glycemic Status Assessment for Patients with Diabetes (HEDIS GSD) | - | Yes | Yes | Yes | - |
| Hypertension: Controlling High Blood Pressure (Quality ID# 236, HEDIS CBP) | Yes | Yes | Yes | Yes | Yes |
| CAHPS Patient Experience | Yes | Yes | - | Yes | - |
Below, you’ll find an archive of prior year quality measures. Click on any year to view and/or download.
Quality Scorecards & Shared Savings
Each year OneCare works with our payer partners to produce annual quality scorecards. These scorecards provide a summary of health care quality across our network of providers. When our provider network performs well on our annual quality measures and reduces cost of care, we have “shared savings” which OneCare distributes back to participating providers. For example, if OneCare has the potential to earn $1.00 in shared savings, but network quality scores are low we may only capture $0.50 of that shared savings. Similarly, outstanding performance on quality measures can offset shared loss. Achieving high scores on annual quality measures is best for patients and allows OneCare to collect and redistribute the greatest amount of shared savings back to our network.
For more information about Vermont’s progress toward achieving the All-Payer Model Agreement targets, click here for reports on the Green Mountain Care Board website.
Capturing Network Performance Spotlight:
OneCare’s Mental Health Strategy – Integrating Quality and Finance
OneCare monitors our network’s performance on mental health care through our nine mental health and substance use annual quality measures. These measures provide insight into current network performance and cover the following domains:
- Screening and Follow Up for Depression in Primary Care Settings
- Follow-Up After Emergency Department Visits for Mental Health or Alcohol or Other Drug Dependence
- Initiation and Engagement in Treatment for Alcohol and Other Drug Dependence
- Follow-Up After Hospitalization for Mental Illness
2. Incentivizing Performance Improvement
Our annual quality measures provide the foundation for OneCare’s quality payment incentive and care delivery improvement efforts. Each year OneCare works with our network made up of participating hospitals, providers, and collaborators across the continuum of care to co-create priorities that align with our mission and our overall quality strategy.
To identify areas for network quality improvement with the goal of improving the health outcomes of Vermonters, each year we:
- Engage our network, board of managers, committees, and workgroups to align with quality improvement work happening around the state and ensure our strategies and practices are informed by representatives across the continuum of care.
- Leverage our unique data set abstracted, compiled, and analyzed by our quality measurement experts to evaluate our network performance relative to national benchmarks and identify opportunities for greatest impact on the health of our population.
- Incentivize selected areas of opportunity through our payment reform programs by linking quality measures to performance-based payments in our Population Health Model program.
Population Health Model Measures
| 2024 Population Health Model Measure | Entities | Measure Description | 2024 Target Rate | Percentile Bench Mark |
|---|---|---|---|---|
| Child and Adolescent Well-Care Visits 3-21 (HEDIS WCV) | Pediatric PC, Family Medicine | The percentage of members 3-21 years of age who had at least one comprehensive well care visit with a PCP or an OB/GYN practitioner during the measurement year. | 61.15% | Medicaid 90th (3-21)* |
| Developmental Screening in the First Three Years of Life (CMS Child Core C-DEV) | Pediatric PC, Family Medicine | The percentage of children screened for risk of developmental, behavioral, and social delays using a standardized screening tool in the 12 months proceeding, or on their first, second, or third birthday. | 57.40% | Medicaid Child Core Set 75th |
| Medicare Annual Wellness Visit | Adult PC, Family Medicine | A yearly check-up for Medicare enrollees assisting participants the opportunity to gain information about their patients, including medical and family history, health risks, and specific vitals. A proactive approach to encourage patients to be proactive about their health and engage in preventive health services. | 51.80% | National ALL ACO Benchmarking - 50th |
| Hypertension: Controlling High Blood Pressure (Quality ID# 236, HEDIS CBP) | Adult PC, Family Medicine | The percentage of patients 18-85 years of age who had a diagnosis of hypertension and whose blood pressure (BP) was adequately controlled (<140/90 mmHg) during the measurement.. | 67.27% | Medicaid 75th* |
| Initiation of Alcohol and Other Drug Dependence Treatment (Quality ID# 305-Medicare)
Initiation of Substance Use Disorder Treatment (HEDIS IET- Medicaid, MVP, PHM) |
Pediatric, PC, Adult PC, Family Medicine | The percentage of new substance use disorder (SUD) episodes that result in treatment initiation and engagement. Two rates are reported: Initiation of SUD treatment (within 14 days) and Engagement of SUD treatment (within 34 days of initiation). | 44.32% | Medicaid 50th* |
| Engagement of Alcohol and Other Drug Dependence Treatment (Quality ID# 305-Medicare)
Engagement of Substance Use Disorder Treatment (HEDIS IET-Medicaid, MVP, PHM) |
Designated Agencies | The percentage of new substance use disorder (SUD) episodes that result in treatment initiation and engagement. Two rates are reported: Initiation of SUD treatment (within 14 days) and Engagement of SUD treatment (within 34 days of initiation). | 18.87% | Medicaid 75th* |
| Follow Up after ED Visits for Patients with Mulitiple Chronic Conditions (HEDIS FMC) | Adult PC, Family Medicine, DA, HHH, AAA | The percentage of emergency department (ED) visits for members ages 18 and older who have multiple high-risk chronic conditions who had a follow up service within 7 days of ED visit. | 58.70% | NCQA National Average Medicare PPO |
| Follow-Up after ED Visit for Substance Use - 30-Day (HEDIS FUA) | Designated Agencies | The percentage of emergency department visits for members 13 years and older with a principal diagnosis of substance use disorder, or any diagnosis of drug overdose, for which there was a follow-up. | 53.44% | Medicaid 75th* |
| Follow-Up after ED Visit for Mental Illness -30 Day (HEDIS FUM) | Designated Agencies | The percentage of emergency department visits for members 6 years and older with a principal diagnosis of mental illness or intentional self-harm, who had a follow-up visit for mental illness. | 73.26% | Medicaid 90th* |
| Follow-Up After Hospitalization for Mental Illness (7 Days) (HEDIS FUH) | Designated Agencies | The percentage of discharges for members 6 years of age and older who were hospitalized for treatment of selected mental illness or intentional self-harm diagnosis and who had a follow-up visit with a mental health provider. | 44.29% | Medicaid 75th* |
Incentivizing Performance Improvement Spotlight:
How Providers May Use Funding from OneCare to Improve Care
Providers are incentivized to add value, not so they can make more money, but so they can provide better care. To offer some examples, a provider can utilize shared savings, funding from Population Health Model, care coordination funding, and/or fixed payment revenue from OneCare to:
- Hire a care coordinator to help ensure their high-risk patients’ providers are communicating with one another about a holistic care plan.
- Employ a social worker to help connect patients with food, housing, transportation, mental health care, etc., as a means of improving their overall health and well-being.
- Incorporate a “lifestyle medicine” nurse practitioner into the practice staffing model to help patients with diabetes make lifestyle changes to lower their blood sugar levels, or to help those at risk of serious cardiac events improve diet, exercise, and stress management.
- Use creative staffing models funded by value-based care to continually improve quality of care, leading to better health outcomes while flattening the cost curve.
3. Quality Improvement Collaborations
OneCare’s quality improvement team works with individual providers, hospital systems, and community partners to create data-driven quality improvement initiatives. OneCare’s quality team offers our partners:
Data Interpretation
Share practice and health service area data to inform local quality improvement work and identify areas of strength and opportunity across the network.
Subject-Matter Expertise
Participate in existing quality improvement efforts led by partner organizations and provide additional leadership capacity as needed to support local initiatives.
Community of Practice
Convene network participants to spotlight local successes, share best practices, and foster a culture of continuous quality improvement
Having OneCare be part of our collective improvement around transitions of care has been invaluable to our community. The Quality Improvement Specialist at OneCare has helped us stay focused on implementing small changes in our systems to make big improvement in transitioning patients from one setting to another.
Quality Improvement Collaboration Spotlight:
Reducing Readmissions in St. Albans
Working closely with members of the St. Albans health service area, OneCare’s Value-Based Care team identified ways that data from OneCare and Northwestern Medical Center could collectively guide improvements in delivery of care. A joint review of data identified hospital readmissions as an opportunity for improvement. OneCare data indicated a particular challenge in readmissions within the first seven days after discharge. Reducing hospital readmissions is one of OneCare’s annual quality measures and also a hospital priority, making it a natural fit for a joint quality improvement project.
The following initiatives were implemented as part of this project:
- A ‘Transitions of Care Committee’ was formed to standardize the process of patient transitions, timely primary care follow-up, and medication reduction.
- The NMC care coordination team established goals and adapted workflows and discharge documentation to support this effort and improve communications.
- The NMC rehabilitation team incorporated changes to their documentation to further facilitate a team approach to discharge planning, optimizing cross-departmental next site of care discussions.
- NMC staff initiated a process change around patient mobility to reduce decline in function during hospital stays to prevent re-hospitalization following discharge.
