Network Performance Management
Through network performance management, OneCare establishes value-based care contracts on behalf of participating providers and supports success under those contracts through prevention efforts, care coordination infrastructure, and quality improvement metrics.
Contracting
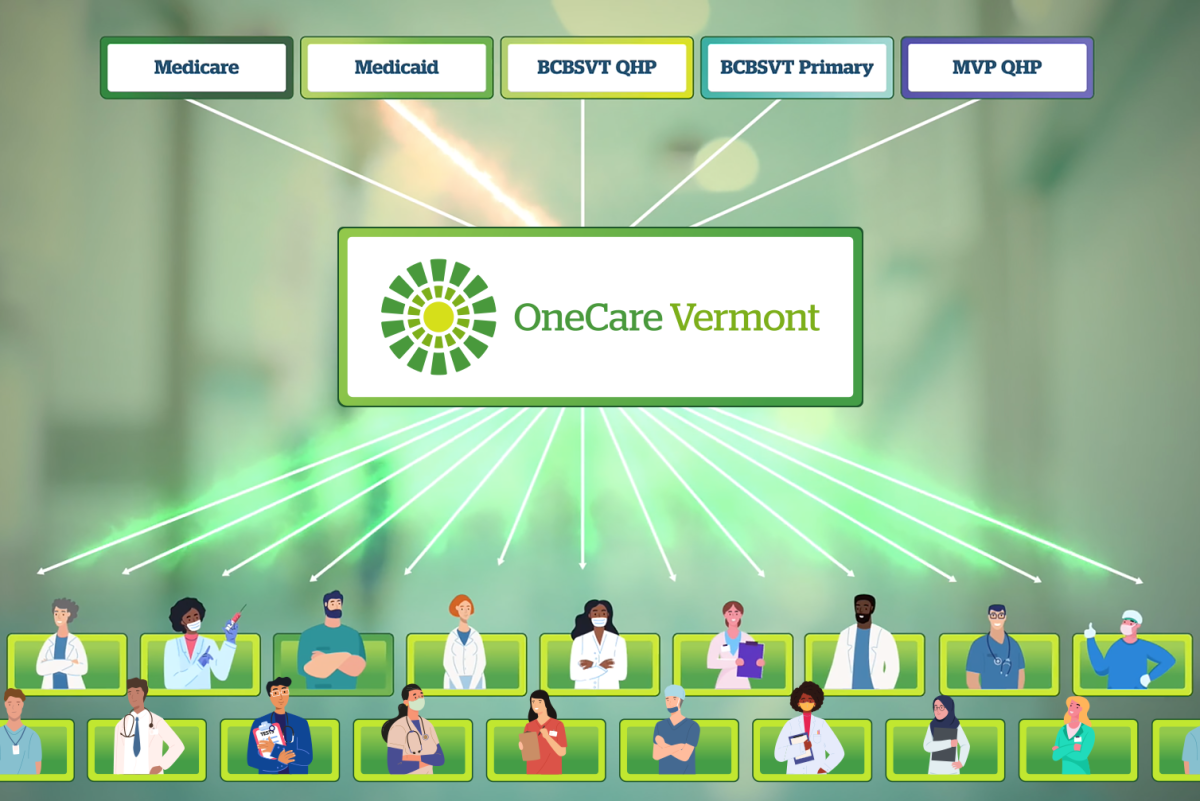
OneCare’s network performance management core capability includes the crucial first step in what OneCare—as an accountable care organization—offers to its participating providers: contracting. OneCare works with Medicaid, Medicare, and commercial insurers to establish contracts for value-based care for its entire network of over 5,000 providers at hundreds of different organizations. OneCare does all the work to navigate the different ways each insurance contract works. Without OneCare, providers would be left to sort all that out with each payer on their own, requiring providers to each hire their own experts to do so and slowing down the progress of value-based care in Vermont.
Care Coordination
OneCare’s care coordination model supports care teams in communities. Care coordination requires a strong relationship between the patient, their primary care provider, and other members of a person’s care team. OneCare provides tools and resources to help facilitate this coordination. With OneCare tools and support, providers work together across organizations to help patients access the care they need and avoid expensive duplicate services. Providers share information about what is happening with the patients they are all caring for—if the person is admitted or discharged from the hospital, if social or economic factors put patients at risk, or if a change in their mental health has occurred. That way, providers caring for the same patient can quickly identify ways to address their needs and the patient only has to tell their story once.
OneCare provides the following to support care coordination:
- Data to help inform primary care providers which patients on their panel may benefit from care coordination
- Best practices and tools for forming a community- and team-based care coordination model
- Secure communication tools care coordination team members can use no matter where they work
- Training for health care workers and partners statewide on care coordination processes and procedure
Fred’s Story: A Case Study of Care Coordination
Quality Improvement
OneCare focuses on the quality of care along with the cost of care. “Quality” in health care refers to the degree to which health care services can increase the desired health outcomes for individuals and populations. At OneCare Vermont, we are building the infrastructure to support and monitor quality improvement efforts across the state.
Network Performance Links to Other Core Capabilities

Core Capability #2:
Data and Analytics
OneCare Vermont makes use of data and analytics by measuring health care cost, quality, and utilization. OneCare measures across an entire population of patients to help providers identify which Vermonters need outreach and which areas of care delivery to improve.
OneCare’s data and analytics support care coordination and quality improvement by identifying patients that could benefit from care coordination and specific quality improvement measures to implement.

Core Capability #3:
Payment Reform
OneCare works with insurers and providers to change how health care services are paid. Under this model, providers can accept regular fixed predictable payments for each patient instead of getting paid for each test or service they perform, and are rewarded based on quality outcomes. When providers are reimbursed for value instead of volume, over time, they can change the way they deliver health care and invest in activities that are designed to lead to better health outcomes—primary care, health prevention, early identification of disease, and the right treatment at the right time.
