The Thomas Chittenden Health Center (TCHC) is an independent family medical practice located in Williston, Vermont, serving over 14,000 patients of all ages. TCHC is part of OneCare Vermont and is committed to transitioning to a new way to pay for and deliver care—one that provides better health outcomes and health care experiences for patients. Approximately 30% of TCHC’s patients are attributed to OneCare’s value-based model, which provides some financial stability while allowing TCHC to focus on improving health outcomes. OneCare Vermont has also provided funding to hire one full-time and two part-time care coordinators to help TCHC’s intensive, high-needs patients, keeping many of them from needing high-cost hospital stays. In 2019, with funding from OneCare Vermont, TCHC developed and initiated a quality improvement project in an effort to improve chronic pain management across the practice.
The Need for Chronic Pain Management Project
The chronic pain management project was led by Rick Dooley, a physician assistant at the practice, in an effort to improve opioid prescribing practices. As Rick puts it, “Providers want to do what is right and better for the patient—they don’t want to prescribe opioids if effective non-opiate alternatives are available. So we decided to look at the structure and see if it supports staff to have time and tools they need to effectively prescribe and manage our patients’ chronic pain.”
It was determined that at TCHC there was significant variability among practitioners prescribing opioids. Since expectations around pain management continually change, TCHC wanted to closely examine opioid prescribing in an effort to find opportunities to improve workflows, ensure consistent understanding of state guidelines, and to implement the use of best practices for chronic pain management. The project sought to create a structure to better support staff with the necessary time and tools to evaluate the need for opioid prescriptions, consider alternative care plans to manage pain, and maintain compliance with state guidelines.
When developing the QI measures that we would track for the project, mental health screening rose to the top. So we took on doing mental health screenings with every patient on chronic opioids. What we found was that underlying diagnoses were getting medicated with the opioids, but when you treated the depression or anxiety with appropriate medications, patients’ physical pain was reduced.
Project Design & Implementation
To start the project, TCHC formed a team that represented every touchpoint a patient with chronic pain might have when interacting with the practice—from initially speaking with a nurse on the phone during scheduling, to seeing a provider. The goal was to create a practice-wide workflow to increase the rate of appropriate screening and treatment goals for chronic pain patients—as well as to increase support for providers prescribing opioid medication. Blueprint for Health provided team facilitation, and the Office of Primary Care and Area Health Education Centers (AHEC) Program provided assistance with coaching. In addition to developing several measures to track quality improvement (QI), a pain management council comprised of primary care providers was formed and met monthly. The council closely reviewed two to three case presentations, each of which included the patient’s history, and then discussed the available treatment options. This aspect of the project was successful, as Dooley stated, “It probably did more to improve our opioid prescribing practices than anything else we did in the project.” With support from fellow prescribers in the University of Vermont’s Office of Primary Care’ s Vermont Academic Detailing Program, the council provided the opportunity for providers to put their heads together and collaborate on the best course of action.
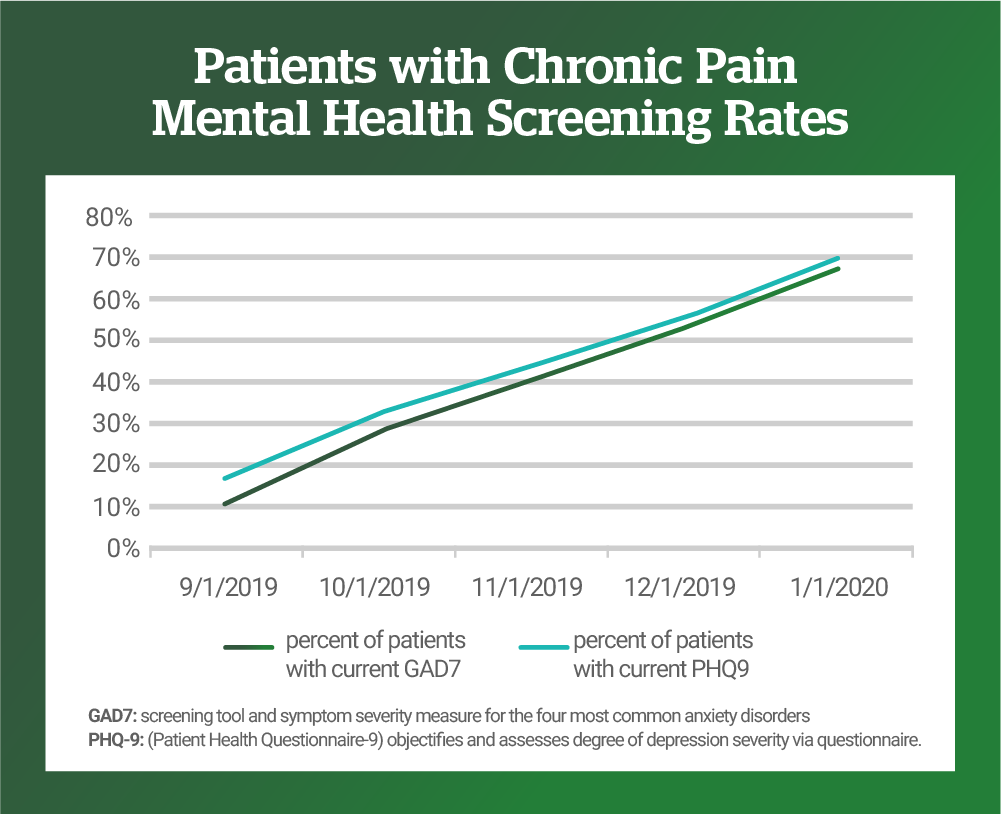
The cultural shift away from opioids in the medical world, and at TCHC in particular, was informed by increased knowledge of how opioids work in the human body to become addictive, as well as an understanding of the link to mental health conditions like depression, anxiety, adverse childhood experiences, and previous trauma. Dooley recalls, “When developing the QI measures that we would track for the project, mental health screening rose to the top. So we took on doing mental health screenings with every patient on chronic opioids. What we found was that underlying diagnoses were getting medicated with the opioids, but when you treated the depression or anxiety with appropriate medications, patients’ physical pain was reduced.” To help Vermonters with chronic pain receive the most appropriate course of care, TCHC increased mental health screening for patients experiencing chronic pain. Screening for general anxiety disorder rose from 10% to nearly 70%, and screening for depression rose from nearly 20% to 70%.
Case Study & Project Results
The success of this quality improvement project is reflected in the case study of a particular Vermonter whose health was directly impacted. The patient was on 250 morphine equivalents over a period of three to four years for a vague chronic pain syndrome. They used to call in frequently, sometimes every week, and often ended up in the emergency department. When their screening uncovered depression and anxiety, the patient was referred to get the proper treatment to care for their mental health. After counseling and in-patient treatment, they are now down to 80 morphine equivalents and are only seen every 90 days for check-ins. Other patients have benefited to some degree from the clinic’s new chronic pain management approach as a result of improved mental care, the introduction of non-pharmacologic treatment options, and changing the structure of the conversation around the patient’s pain. These patients have been able to achieve improvements in overall functionality and also reduce opioid intake.
Overall, the pilot project from September 2019 to January 2020 showed encouraging results. In addition to the marked increase in the screening rates for underlying anxiety and depressive disorders, other prescribing strategies such as implementation of surveillance urine drug screenings, annual treatment goals, and writing prescriptions in seven-day increments to avoid weekend refill requests increased notably. There was also an increased sense of support and collegiality among the prescribing physicians, physician assistants, and nurse practitioners. Nurses and support staff reported improved comfort with management of chronic pain patients because of the newly consistent workflow. In addition, while a reduction in opioid prescribing was not the stated goal, there was a reduction in the number of opioid prescriptions at TCHC from 466 to 424, a reduction in number of people with chronic pain who were prescribed opioids from 355 to 347, and the number of patients prescribed both opioids and benzodiazepines, also highly addictive, went from 110 to 100. When comparing overall 2018 to 2019 annual morphine equivalents prescribed, TCHC saw a reduction of 22%.
%
reduction in annual morphine equivalents prescribed 2018 to 2019
Project Connection to OneCare Vermont Mission
TCHC’s quality improvement project clearly had high-impact on the health and well-being of patients in their care. The project also helped create a sustainable process for the practice that has continued past the reporting-period for the project and has provided a template for future improvements in quality. It also highlights an important connection between the work of health care practices to the broader mission of OneCare Vermont. The funding received from OneCare allowed the practice to offset lost time and revenue when they weren’t seeing patients because of both the time needed to administer the project, and also to participate in the pain management council. The funding also allowed providers to spend more time with patients and perform mental health screenings. There is more opportunity for innovation when a practice isn’t dependent on counting every patient visit or service for income, but is instead able to operate under a set, predictable, and fixed budget supplemented by OneCare in order to better serve patients with higher quality care, and to even be able to receive additional funding when certain improvements are made.
Thomas Chittenden Health Center was also featured in a September 1, 2020 case study by the Commonwealth Fund.
For more information:
Please contact Public Affairs at OneCare Vermont. public@onecarevt.org | 802-847-1346
To stay up to date on OneCare, please visit our news blog and our social media channels on LinkedIn and Twitter.
