In 2020, Mathematica, on behalf of the Centers for Medicare and Medicaid Services (CMS), closely examined OneCare’s community-based care coordination program, aimed at helping Vermonters who are considered high (or very high) risk “because of their historical cost and utilization of health care.” CMS/CMMI has recently published a case study that describes the development, implementation, and the initial results for this program.
OneCare’s care coordination program is designed to encourage and facilitate coordination across a range of providers and service organizations in specific services area in order to better meet the health needs of Vermonters and improve outcomes. Examples of providers and organizations include primary care providers, mental health agencies, congregate housing staff, home health providers, and area agencies on aging.
The case study revealed that “… [OneCare Vermont] reported not only an increase in primary care engagement among beneficiaries who participated in the program but also reductions in emergency department utilization and costs. OneCare Vermont’s approach to care coordination may be informative for ACOs and other health care organizations that are designing programs intended to foster collaboration among primary care, specialty, and other community-based providers.”
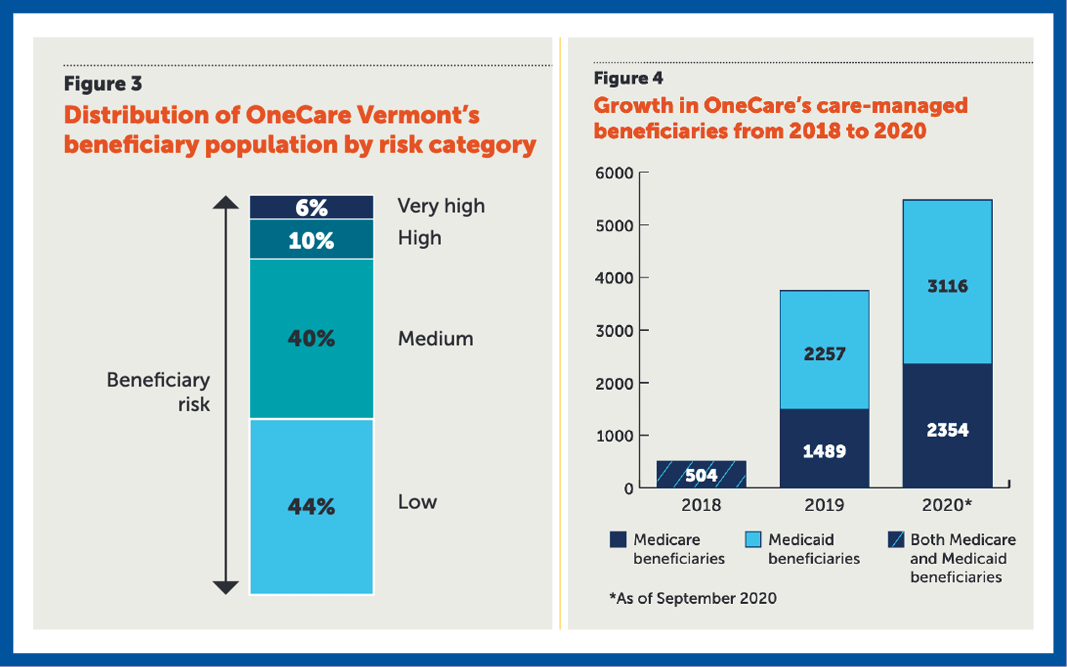
Pictured above: two figures from the case study. Figure 3 reflects the range of risk distribution from low to. very high risk, and figure 4 shows the growth in the number of beneficiaries who were care-managed since the inception of the care coordination program in 2018.
Depending upon the patient’s medical history and the challenges that they’re experiencing, the care coordinator will wrap the right team around the patient.
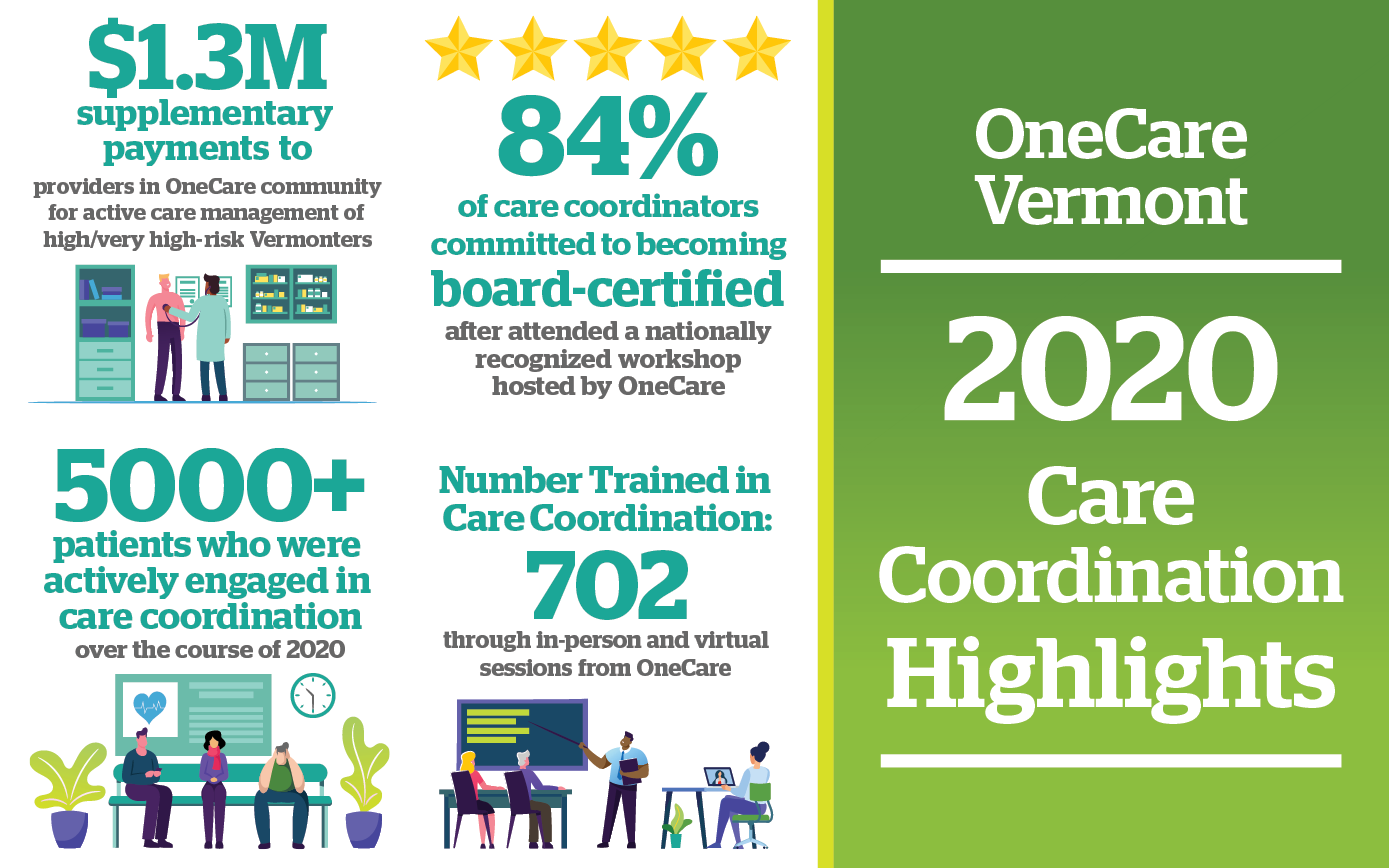
Pictured above: Additional highlights of OneCare’s care coordination program in 2020, via OneCare.
More about ACOs
The Centers for Medicare and Medicaid Services (CMS) through their Innovation Center (CMMI), supports the development and testing of innovative health care payment and service delivery models. These models are designed to encourage health care providers to coordinate more effectively to deliver value-based care to their patients, which means rewarding providers based on the patient’s health and quality of care delivered. One way that CMS attempts to accomplish this, is through their Accountable Care Organization Models. OneCare Vermont is one such ACO, designed to deliver high quality care to Vermonters through the Vermont All-Payer Medicare ACO Model.
For more information:
Please contact Public Affairs at OneCare Vermont. public@onecarevt.org | 802-847-1346
To stay up to date on OneCare, please visit our news blog and our social media channels on LinkedIn and Twitter.
